Author: Abhishek Dash
This is no longer a secret: the Coronavirus pandemic will forever change how we live and work. The level of efficiency, as well as the speed we adapt to the new environment, will depend on our understanding of the problem. It will also help determine how suitable and efficient the proposed solutions will be.
In this pandemic, population density is a factor that determines how vulnerable places are to the virus. Across the world, Covid-19 has hit hard in several locations such as factories, places of worship, and sports stadiums. The most hard-hit areas are large, densely populated cities like New York, Milan, and London. The cities have large flows of visitors and tourists, diverse global populations, and dense residential areas.
A person breathes in 14,000 liters of air per day. The presence of contaminants in the air we breathe in can result in adverse effects on people’s health.
Brief Scientific Facts About Coronavirus
How does the Coronavirus spread?
The Coronavirus becomes airborne when an infected person expels respiratory droplets by coughing, breathing, and even speaking. These smaller droplets can carry and spread the virus. There are mainly two exposure mechanisms[1][2]:
- Close contact transmission through large droplets (> 10 microns), which are released and fall to surfaces less than about 6ft from the infected person. Droplets are formed from coughing and sneezing (sneezing forms many more particles typically). Most of these large droplets fall on nearby surfaces and objects – such as desks and tables. People can catch the infection by touching these contaminated surfaces or objects; and then touching their eyes, nose, or mouth.
- Airborne transmission through small particles (< 5 microns), which may stay airborne for hours and can be transported long distances. This mechanism implies that keeping 6 ft. (2 m) distance from infected persons might not be enough. Infection risk can be high in crowded and poorly ventilated spaces. The coronavirus particle can remain active in common indoor conditions for up to 3 hours. Such small virus particles stay airborne and can travel long distances carried by airflows in rooms or in the return air ducts of ventilation systems. Using toilets can also pose a risk because when a toilet is flushed, air plumes containing droplets and droplet residue can spread in the air. It is important to flush the toilet with the lid closed!
How Does Air Move in a Building?
An understanding of air movement in buildings is essential when investigating pathogens, such as the Coronavirus. Airflow patterns in buildings are the result of combined forces such as wind, the stack effect or called chimney effect[3], distribution systems, and ventilation mechanisms. With COVID-19, the airborne transmission through exposure to small droplet particles has currently been acknowledged by WHO for hospital procedures and indirectly through the guidance to increase ventilation[4]. Nishiura et al. 2020 analyzed superspreading events, which showed that closed environments with minimal ventilation strongly contributed to a characteristically high number of secondary infections.
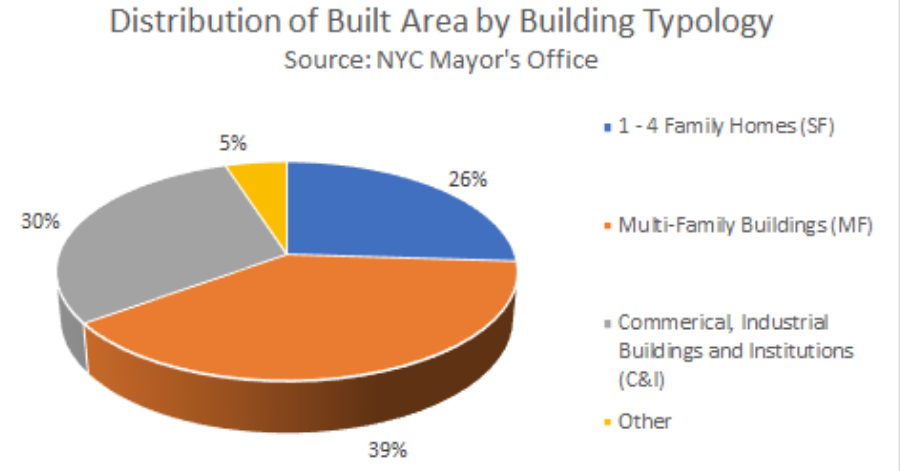
Based on the building typology in NYC, typical air distribution systems in buildings can be categorized into four types shown below.
What are the common issues and how can we prevent the spread of COVID-19 in buildings?
Smeiszeck, Lazzari, and Salathe (2019) found that ensuring even minimum levels of outdoor air ventilation reduced influenza transmission as much as having 50 percent to 60 percent of the people in a building vaccinated.
Most single or two-family homes (SF) homes do not have ways to regulate outdoor air intake through HVAC systems, and as a result have to rely on operable windows to bring in outdoor air in buildings that help dilute airborne contaminants, making infection less likely.
Commercial and common areas of large multi-family buildings typically recirculate some air. This has been proven to lead to a higher risk of infection during outbreaks, as contaminated air in one area is circulated to other parts of the building (as it did in the school with measles). Underventilation frequently occurs if the system is not arranged to introduce at least a minimum quantity (as opposed to percentage) of outdoor air as the variable air volume (VAV) system throttles back from full airflow, or if the system supply air temperature is set too low for the loads present in the zone. When it’s very cold or very hot, the air coming out of the vent in these buildings may be completely recirculated. That’s a recipe for disaster.
A review study touches on indoor humidity playing a surprising role in curbing the spread of the virus because dry air impairs a person’s ability to fight off respiratory viral infections. Low humidity also impairs the host’s ability to clear airborne viruses from their nose without getting infected, a fairly gross process of clearing snot from your nose (officially, it’s called mucociliary clearance). This is why you may find humidifiers to be helpful if you have sinus or breathing issues. With viral seasonality being a factor public health experts predict, indoor humidity plays a role in decreasing seasonal disease transmission. In humid conditions, these tiny droplets don’t evaporate as much, so they drop down more quickly than they would in dry conditions. Virus-containing droplets that travel farther in drier air are more likely to infect a new host. However, indoor humidification is not common in most HVAC system designs, largely due to equipment cost and maintenance concerns related to the risk of over humidification increasing the potential of mold growth.
Here’s what we should be doing. First, bringing in more outdoor air in buildings with heating and ventilation systems (or opening windows in buildings that don’t have these systems) helps dilute airborne contaminants, making infection less likely. For years, we have been doing the opposite: sealing our windows shut and recirculating air.
In relation to buildings with dedicated ventilation systems (not mechanical ventilation), it is recommended to switch on ventilation systems a couple of hours earlier and to extend the operation. A better solution is to keep the ventilation on 24/7, possibly with lowered (but not switched off) ventilation rates when people are absent in order to remove virus particles out of the building. Local Exhaust ventilation (LEVs) systems of toilets and bathrooms should always be kept on 24/7, and make sure that negative air pressure is created to avoid fecal-oral transmission.
This blog post also includes the hypothesis for how indoor humidity may help reduce viral transmission. A 40% to 60% relative humidity may be ideal to reduce viral transmission and infection in general, and increasing evidence indicates that higher relative humidity has been shown to reduce infectious influenza virus in simulated coughs[5]. While administrators and building operators should consider the costs, merits, and risks of implementing central humidification, especially during new construction or as a retrofit, it may be too time-intensive to implement in response to a specific viral outbreak or episode. In addition, increased relative humidity (RH) may lead to increased buildup on filters, decreasing airflow. However, in pandemic situations, this practice likely increases the effectiveness of capturing viral particles, and this benefit outweighs the increased filter maintenance required. Therefore, targeted in-room humidification (room humidifiers) is another option to consider, and this may reduce the likelihood of a maintenance oversight causing over humidification.
What’s the link to COVID-19 mortality in the worst affected areas?
We knew that COVID-19 adversely affects patients with pre-existing conditions. We now are aware that patients in areas that had high levels of air pollution before the pandemic are more likely to die from the infection than patients in cleaner parts of the country, according to a new nationwide study that offers the first clear link between long-term exposure to pollution and COVID-19 death rates. The results suggest that long-term exposure to air pollution increases vulnerability to experiencing the most severe Covid-19 outcomes. The burden of air pollution is not evenly shared. Poorer people and some racial and ethnic groups are among those who often face higher exposure to pollutants and who may experience greater responses to such pollution[6]. There is also a greater risk of particle pollution coming from traffic sources where residential segregation based on housing market dynamics and land costs has led to the aforementioned groups witnessing higher rates of: asthma attacks in children and the onset of childhood asthma, impaired lung function, premature death and death from cardiovascular diseases and cardiovascular morbidity[7].
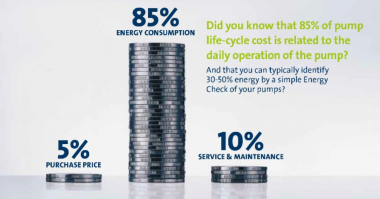
To address the concern about air quality in one’s buildings, one can minimize cross-contamination by enhancing the level of filtration. Most commercial, institutional buildings use low-grade filters that may capture less than 20 percent of viral particles. Most hospitals, though, use a filter with what’s known as a MERV rating of 13 or higher. And for good reason — they can capture more than 80 percent of airborne viral particles. For buildings without mechanical ventilation systems, or if you want to supplement your building’s system in high-risk areas, portable air purifiers can also be effective at controlling airborne particle concentrations. Most quality portable air purifiers use high-efficiency particulate absorbing (HEPA) filters, which capture 99.97 percent of particles. There are some instances when far-UVC light with wavelength around 220 nm (safer for humans), could be incorporated into conventional light fittings so that they would be very easy to install in public spaces like schools, airports, train stations, airplanes, and hospitals, common areas/lobbies of buildings to limit the spread of the virus that causes COVID-19 as well as other coronaviruses that cause other respiratory diseases. Currently, a couple of companies have developed practical inexpensive far-UVC lamps and a US lighting fixture company is incorporating the far-UVC lamps into conventional light fittings.
Who are the key stakeholders here and what can they do?
There will be a need for large-scale social orchestration between different stakeholders that include government agencies, real estate companies, and portfolios, landlords, tenants, construction managers, engineers, architects, and various community organizations that own/operate/maintain/live/engage in the built environment.
To start, the industry must create a COVID task force that focuses on developing strategies, galvanizing resources, and coordinating efforts in response to the short and long-term impacts of the pandemic on buildings and its residents – from information dissemination to system-wide service provision to federal policy support- is essential. The creation of this task force will provide a mechanism to focus on this immediate challenge and collect and apply the expertise of our global community, which includes practicing physicians, environmental and behavioral scientists, leading design practitioners, and innovation leaders from global corporations.
From a policy standpoint, utilities and municipalities can advance health and well-being by enacting local laws that promote healthy building standards and best practices. These standards should form new guidelines for Prevention and Preparedness, Resilience and Recovery for individuals, organizations, and communities to help them better integrate actionable insights and proven strategies into how they manage both their buildings and their organizations.
ASHRAE, a professional society for HVAC personnel, released their position on infectious aerosols, and released Guidance for building operators during the COVID-19 pandemic. It’s a comprehensive list of recommendations for different building sectors and scenarios. For e.g., there’s guidance for single-family and multi-family homes, and guidance on how to create and isolate a place to protect high-risk individuals. The WELL Building Standard is a good primer about air quality management, building operations & maintenance, and design programs so as to work more effectively and efficiently to prevent and solve the health problems. Using best-practices from these resources and enacting a plan for buildings to follow/abide by is necessary to prevent transmission of pathogens through our buildings.
References:
1. Luongo JC, Fennelly KP, Keen JA, Zhai ZJ, Jones BW, Miller SL, 2016. Role of mechanical ventilation in the airborne transmission of infectious agents in buildings. Indoor Air 25(6): 666-678
2. Li Y, Huang X, Yu ITS, Wong TW, Qian H, 2005a. Role of air distribution in SARS transmission during the largest nosocomial outbreak in Hong Kong. Indoor Air 15(2): 83-95.
3. Chimney effect, where warm air rises and cool air falls, may be increased by building shapes, natural chimneys such as stairwells or elevator shafts, and building exhaust ventilation systems.
4. WHO, 2020c. World Health Organization, Coronavirus disease (COVID-19) technical guidance: Guidance for schools, workplaces & institutions. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technicalguidance/guidance-for-schools-workplaces-institutions (Retrieved March 21, 2020)
5. Noti JD, Blachere FM, McMillen CM, Lindsley WG, Kashon ML, Slaughter DR, Beezhold DH. 2013. High humidity leads to loss of infectious influenza virus from simulated coughs. PLoS One 8:e57485. doi:10.1371/journal.pone.0057485.
6. Disparities in the Impact of Air Pollution, American Lung Association, Clean Air, Clean Air Outdoors, Who Is at Risk
7. Living Near Highways and Air Pollution, American Lung Association, Clean Air, Clean Air Outdoors, Who Is at Risk



Comments